Just over a week ago I got a text message from a friend asking for prayers. His wife was being induced at 35 weeks due to low amniotic fluid.
My first thought?
Oh crap. She's gonna end up with a c-section. Yet another friend to "welcome" into the Sisterhood of the Scar.
Turns out, I was wrong. Even though she was induced at the hospital with the 3rd highest cesarean rate in the Twin Cities (30%), she escaped a surgical birth.
How did this happen?
I bumped into her at church this morning. She told me that she was freaked out when she knew she was headed for induction. She had the same thought I did, that she was probably going to end up with a cesarean. The chances were certainly good - a high risk situation, induction, a preemie on the way...
I think it was her preparation (and no doubt support of her husband and others) that made a huge difference. This was her second birth. Her first had been at the same hospital, but they were well-prepared the first time, too. They had taken Bradley classes and stayed home as long as possible during labor. She had a drug-free birth the first time around. That same mindset and preparation helped her avoid more interventions during her induction this time. She told me, "The only bummer was that I had to be in the bed the whole time [for monitoring, Pitocin, etc]. But I used having to go to the bathroom a lot as my excuse to get up often. So, I got the drug-free birth I wanted. Well, except for the Pitocin...."
My friend was prepared to meet the challenges of an unexpected, stressful birth because she knew from experience as well as from childbirth eduction that sometimes you have to work with what you've got. She knew that moving around is so important in labor. So, she used a little trick to work the system and get up as much as she could. It wasn't a completely ideal situation, but she worked for the birth she wanted even despite the odds.
Sunday, January 31, 2010
Sunday, January 24, 2010
What to Say, How to Say It
I just wanted to ponder the issue that a lot of us at ICAN have run into. And that is -how to present/give birth advice in a way that people will listen, not be offended, not go in the wrong direction, and again - actually listen and take in what you have to say.
Let's face it - most of us are a part of ICAN because we have been affected by birth in one way or another. (If you just happen upon this blog or are passing by - welcome!). I also think that most of us find opportunities all of the time to inform others about birth. Some people ask for suggestions, and there are others who are just talking about their pregnancy or birth and we can't seem to keep our mouths shut - I mean - it would be a sin to withhold all of the information we have.
I ponder this topic because the last thing I want to do is turn someone off so much that they won't even listen to what I have to say. And I must say, my approach has changed a lot over the past couple of years. There was a time when I would just jump in and say things when my advice wasn't asked - ie) "Don't induce 1 week past your due date - inductions are horrible - let your baby stay in ." - to a 2nd time mom that had a vaginal birth her first time.
I'm still struggling with the right balance. Just recently I made it known, subtly, to someone I have to see daily, that I don't exactly agree with weekly cervical checks from 36 weeks on out. I'm kind of wishing I would have just kept my mouth shut. Yet, I know I've slowed down more, listened more, and have gotten better at trying to put information out there in a factual, somewhat non-biased sounding way. I really try to affirm actions and decisions that seem informed by mothers. I seek to encourage and uplift all mothers regardless of whether or not I agree with them. I have to remember that the last thing that I want any mother to feel is put down by what I say - because that is the opposite of what we are trying to do. Sometimes my passion for wanting the best for all mothers and babies is without inhibitions.
So, tell me - what is your best approach with pregnant mothers and birth advice? Or perhaps, share an instance that you regret and wish you could have approached differently. I'd love to hear people's tactics for giving information in a sensitive way - yet with the mission towards better birth in mind.
Let's face it - most of us are a part of ICAN because we have been affected by birth in one way or another. (If you just happen upon this blog or are passing by - welcome!). I also think that most of us find opportunities all of the time to inform others about birth. Some people ask for suggestions, and there are others who are just talking about their pregnancy or birth and we can't seem to keep our mouths shut - I mean - it would be a sin to withhold all of the information we have.
I ponder this topic because the last thing I want to do is turn someone off so much that they won't even listen to what I have to say. And I must say, my approach has changed a lot over the past couple of years. There was a time when I would just jump in and say things when my advice wasn't asked - ie) "Don't induce 1 week past your due date - inductions are horrible - let your baby stay in ." - to a 2nd time mom that had a vaginal birth her first time.
I'm still struggling with the right balance. Just recently I made it known, subtly, to someone I have to see daily, that I don't exactly agree with weekly cervical checks from 36 weeks on out. I'm kind of wishing I would have just kept my mouth shut. Yet, I know I've slowed down more, listened more, and have gotten better at trying to put information out there in a factual, somewhat non-biased sounding way. I really try to affirm actions and decisions that seem informed by mothers. I seek to encourage and uplift all mothers regardless of whether or not I agree with them. I have to remember that the last thing that I want any mother to feel is put down by what I say - because that is the opposite of what we are trying to do. Sometimes my passion for wanting the best for all mothers and babies is without inhibitions.
So, tell me - what is your best approach with pregnant mothers and birth advice? Or perhaps, share an instance that you regret and wish you could have approached differently. I'd love to hear people's tactics for giving information in a sensitive way - yet with the mission towards better birth in mind.
Saturday, January 9, 2010
Jamie's Breech Birth Story
On April 1, 2008, I found out that Baby (gender at the time was unknown) was breech. Approaching 33 weeks pregnant, I was unafraid because I knew there was plenty of time for Baby to turn around. For curiosity's sake, I posed a question in an online community, asking what typically happens if a woman goes into a hospital in labor with a breech presenting baby. The answers I received were, to say the very least, shocking, eye-opening and frightening. I had women point me in the direction of "Pushed" by Jennifer Block in which there is at least one story of a woman forced by court order to have a c-section against her wishes because her doctor thought it best for her particular situation. The general reply I received from the women in their replies was that to refuse a c-section would be unwise since most all doctors nowadays are not taught the art of breech vaginal delivery. Many were helpful, offering links to Gail Tully's "Spinning Babies" website, as well as ICAN. I was told about the various techniques to help coax a breech baby to turn. To be honest, I didn't follow any of the advice or techniques yet, Baby was once again head-down by April 7, 2008.
I didn't worry about it and, in fact, I went to that same online community and did a little online happy-dance and bragged that Baby had resumed a vertex position. If I'd only known...Toward the end of my 37th week of pregnancy, May 5, 2008, I went in for my weekly appointment with my midwives at a large hospital in Minneapolis. She laid hands on me and got a strange look on her face and said something about breech presentation. She left the room and returned with a portable ultrasound machine. I held my breath as the midwife spread the lovely goop on my belly. BAM! There was a little head pushing into my ribcage where there was supposed to be an ass. I was not amused. My midwife was going to schedule an external cephalic version (ECV) but by the time we were finished with my appointment, the scheduling office was closed. She spent a lot of time with me showing me various positions to get in to to coax Baby to turn and gave me other tips as well; much along the same lines as what can be found on the Spinning Babies website. She also made an appointment for me to have a moxibustion session later that week. Moxibustion is a traditional Chinese medical practice that involves the burning of herbs to stimulate acupuncture points. In pregnancy, the herbs are burned near the pinkie toe on the woman's foot. When I finally did get in to have a session, it was just for the woman to show me how to do it myself at home. I went to my mother's house and had her do it for me and it was quite surreal. It certainly did get Baby moving around a whole lot but all that movement was a whole lot of nothing and Baby still remained breech. The session did make for a neat video to add to the story! I swear, it was like something out of the "Aliens" movie! I wasn't able to get the supplies needed for the moxibustion until what turned out to be 2 days before I gave birth. The session had been scheduled for the middle of my 38th week of pregnancy but the night before I was supposed to go in, I got a call from my surgeon's office saying a surgery I'd previously been turned down for due to my late stage of pregnancy, was back on. So the moxibustion was canceled and instead I spent the better part of the day on an operating table getting my right hand sliced open for the second time during my pregnancy in order to repair a tendon injury. Because of this surgery, I was unable to do the water therapy I'd wanted to try to get Baby to turn. I did go to the pool on Mother's Day (I even got in for free!) but I had a splint on my hand and could not go underwater so it was all but pointless, at least from the point of view of someone attempting to get a breech baby to turn.
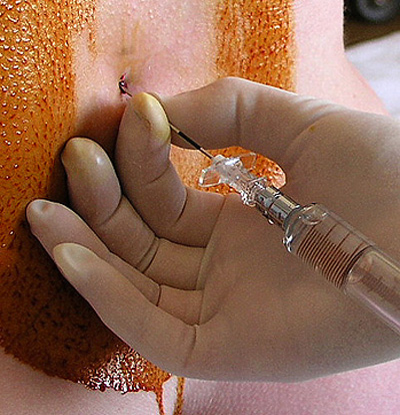
I had 2 versions performed during the last week and a half of my pregnancy. The first one was at the hospital. I went in early in the morning and was placed in a triage area of the maternity ward surrounded by other women in various stages of pregnancy. I laid in the bed hooked up to an IV for fluids and a fetal heart rate monitor for about an hour and a half before they brought me into the ultrasound room with the OB who attempted the version. The lights were kept low as a technician stood by and checked periodically with the goop-covered transducer to see if any progress was being made on Baby's position. Let me tell you, if you think having a human kicking its way around in your uterus is a strange feeling, try having someone on the outside attempt to get that tiny human to move in a direction it does NOT want to go. I walked around for days afterward feeling as though I'd been punched repeatedly in the stomach. I left that day feeling sad and defeated.
That weekend I networked in a way I never had before. I called my aunt who gave me the number to my other aunt who gave me the number to a home birth midwife that she had met through some group or other. I called the midwife and left a voicemail, practically in tears, and let her know of my situation. She called me back the next day and we talked some things over. She said that she would gladly have me come to her house and she would make another attempt at a version. It was a Monday morning when my boyfriend and I drove to her home in St. Paul. I ran into a friend of mine in the lobby of her building and he got a kick out of my story behind being there in his building! The midwife buzzed us in and when we walked into her apartment, I felt very welcomed. Her kids were running around playing and were very respectful of the fact that Mommy was with a client. They just kind of played off to the side while the midwife and her assistant laid hands on me while I was laying on a mat on her carpet. She was very gentle and despite still feeling bruised from the hospital's attempted ECV, I didn't feel any pain. The assistant listened with the fetoscope while the midwife worked. She must have had her hands on me for 10-15 minutes before she finally gave up and let me know that this baby was wasn't going to turn. She told me she was not going to charge me anything for the attempt, which was a welcomed silver lining amidst a sea of mucky grey.
She then offered to attend my birth at home. The thought hadn't occurred to me, though I had been told that was about the only way to accomplish a vaginal breech delivery. If I knew then what I know now, I would have jumped at the chance. To be honest, that little voice in my head told me to have my birth with her and I really did want to despite knowing virtually nothing about home birth, especially considering my first birth was a stereotypical hospital birth with an epidural and a midwife I'd never before laid eyes on. But I really knew I could trust this midwife. However, after discussing it with my boyfriend and my mother (I'd be giving birth at her house if that's the route we took), they were not comfortable with the idea therefore the midwife was not comfortable since they were my support persons.
So there I was, 9 months pregnant and knowing I was going to have a c-section despite the fact that women have been birthing babies who present in all forms of presentations since the dawn of time. It sounds extreme but it was like a death sentence for me, the c-section, I mean. I had done everything I could think of to get Baby to turn. I spent so much time inverted hanging off the end of my couch that upside-down began to look like right-side-up to me. I talked to Baby so often that I thought for sure it would be born so sick of my voice that it would cry whenever I spoke. I played music via headphones between my legs while holding a cold pack on baby's head near my rib cage. I tried a heat pack in place of the head phones. My best girlfriend had brought me her Ab Lounger that allowed me to get into an even better inverted position than I was able to accomplish on my couch. I watched a lot of TV upside down with a cold pack on my ribs and a heat pack and headphones down below while I sang little songs to Baby about how it needed to go toward the sound and flip around for Mommy.
At 39 weeks exactly, I had my last midwife appointment. My favorite midwife was there that day and she had no choice but to send in an OB who told me all of the scary stories about why my wanting to have a vaginal delivery could very well kill me and my baby. She brought in copies of statistics and studies (I know now that this was excerpts from the Hannah Term Breech Trial that has since been proven to be so full of holes that it's almost laughable that a medical professional was showing them to me) and I read through them while listening to her and this little voice in my head was telling me to run very very far away. But at that point, I didn't have a choice. I'd called all the area hospitals and no one would accept me for a vaginal breech delivery. A nurse at one hospital I called went so far as to lay into me about how unwise of a choice I was making by trying to have a vaginal breech delivery. I think I simply hung up on her. In general, I got the same tone from every place I called.
I didn't give up trying to call to find a provider but I had no luck. Finally I was at a coffee shop near my house writing up a new c-section birth plan when my favorite midwife from my hospital called me. She said she'd just left a conference and met a perinatologist from a different hospital who wanted to meet me for a consult the following day. She got his office on the phone via 3 way and I went to the consult the next day.
During the consult, I was told that in the practice of 15 doctors, 12 would be open and welcoming for my vaginal delivery, but that 3 would push strongly for a c-section. He basically said that, while those 3 would push for the surgery, they were ALL more than trained and competent enough to do a vaginal delivery. He made sure I knew the risks but made it clear that he felt those risks only really applied to women with larger babies and who had not given birth before. He didn't warn me in a frightening way that the choice I was making was going to harm me or my baby. He did say there was a risk, but also said there were many risks to c-sections and said that if there was such a thing, I was a perfect candidate for a breech vaginal delivery. He did a quick ultrasound which showed Baby was 6 pounds even and he told me what to do when I was in labor.
I laugh now when I think of the conversation I had with him that day. He said just in case I came in in labor to one of the 3 doctors that would push for surgery, to labor at home as long as possible and to only come in when I felt I was very far into labor. Overall, he made me feel really calm. Well, that was the calm before the storm I suppose, but I'll get to that later.
My labor had kind of started that Monday, when I was 39 weeks along. Contractions were regular but they were 15-19 minutes apart, though slowly getting closer together. I knew I wasn't going to make it to the end of the week. I drank a few glasses of wine over the course of those few days before I had my consult with the perinatologist because even though I'd accepted that I had to have surgery, I almost knew I wasn't going to have to; the same little voice that told me a c-section was not the "right" thing for me also told me to have faith. No sooner did I get home from the consult than my contractions started to pick up. By 9pm that night they were 7 minutes apart and getting closer. I got no sleep that night. I'm not comfortable sharing the story of my labor that night because it's pretty much littered with personal drama, for lack of a better way to put it. My boyfriend never really saw me in labor with our first daughter, not TRULY in labor. With her, my water broke, we went to the hospital, got the epidural when contractions started and I pushed her out in 47 minutes, there was no primal woman in labor going on as there was with my breech baby. With my breech baby, it was a lot more primal, I was listening to my body, I was having contractions to signify I was really in labor and labored at home as opposed to having waters break and immediately going to the hospital. I was a lot more in touch with myself as a mom, and as a pregnant woman and I think I must have been like a complete stranger to him and he was not there for me in any sense.
By around 2pm the next day, I'd been up all night walking the sidewalk in front of my place. Mike's mom came over that morning and had spent a good portion of the night talking to me on the phone. I was living next door to my mom's house so my mom was there as well as my best friend. Mike was at home right next door but I don't think I saw him until hours later when we were all getting ready to go to the hospital and, to be honest, I didn't care. I was deliriously in love with being in labor; I can't think of a better way to describe it. It was beautiful; everything I'd read about in Ina May Gaskin's books. I felt so empowered and beautiful and I laughed through the (quite painful) contractions as I dropped to my knees to moo like a cow or blow raspberries. During a late lunch, my mom and Mike's mom realized that my contractions were barely over a minute apart and they convinced me it was time to go to the hospital. I agreed about half an hour after that; it was around 3 in the afternoon.
I don't remember a whole lot about the ride to the hospital aside from arguing with my mom for going over bumps in the road because it made my contractions unbearable. Since I'd just switched practices the day before, I didn't have any idea where to go once I got to the hospital. I tried calling 411 to get the number to the hospital but a woman in active labor strapped behind a seat belt, mooing like a cow and arguing with her mother does not lead to a successful phone call. We just parked in the ER parking lot and were directed to the maternity ward. The walk down the hallway and the ride in the elevator is a complete blur to me of leaning against walls and I think I may even have sat on the floor once or twice. I was still laughing. I feel like the perinatologist who did my consult really set my mind at ease and despite the fact that I was going to be giving birth in a hospital again, I felt at peace because I knew I was going to get the safe, vaginal breech birth I knew I and my baby deserved.
Of course, I wound up with a doctor who wanted to do a c-section. I had a huge fight with the doctor and kicked him out of my room and said if he wouldn't do it, to find someone who would. He left and came back 45 minutes later with what I love to call the "waiver of baby death" and said that while he was uncomfortable doing it, he was probably one of the most trained for breech delivery, having been in practice since the mid 70's when breech delivery was a normal thing. During that 45 minutes that he was out of the room (and I was in the sterile maternity intake room hooked up to monitors laying flat on my back, of course), my labor all but stopped. Mike was nowhere to be found because he'd found other more important things to tend to like locking his keys in the car outside the hospital. My contractions became unbearably painful and according to my mom and Mike's mom, I was losing it completely; hyperventilating, crying, shaking, angry. While I calmed down after he agreed to "allow" me my vaginal delivery (gee, how generous of him, right?), I never did regain that sense of peace and calm I'd had when laboring at home. I think that's why I finally broke down at 7pm or so and got the epidural. It wasn't really for the pain, which I was managing quite well again at that point. I was more than afraid the doctor would find a "reason" to do the surgery and I did not want to risk there not being enough time and my having to use general anesthesia.
I basically gave up. I don't blame myself for it, but I know I gave up. I let him break my waters and I let him administer Pitocin. I did have a LONG conversation with him about not wanting to have him perform an episiotomy during the pushing stage, that I knew my body could push Baby out without one and that if it came down to it, I'd rather tear along the path of least resistance. Just shy of 2am, I felt that burning feeling and I knew from my previous birth that I was ready to push. That's when it got crazy...I was wheeled in to the OR (I already knew I'd be giving birth in there, which was kind of frightening) and there I was, Mike was the only person allowed in the room, covered head to toe in a gown and mask, holding the video camera. I don't remember exactly how many people were in the room but they had the doctor's surgical team and the NICU team in there with us. I don't remember exactly how long it took to push her out but I know it had to have been less than 10 minutes because I had her out with the 3rd contraction. After the 2nd contraction, he asked the nurse for the tool so he could do an episiotomy and I screamed out NOOOOOO. He told me her heart rate was dropping and that he needed to get her out RIGHT AWAY. Of course I went with it. She was born at 2:04am on May 16th 2008. Six pounds 3 ounces of perfection. I was able to hold her immediately while he stitched me.
I left after she was 12 hours old, much against medical advice. I knew I wasn't going to stay as long as they wanted me to but I left so soon because the pediatrician came in when she was around 10 hours old or so and before asking me how I or she was doing, he said he'd taken a look at my chart and saw that I was still nursing my 19 month old and that I should probably stop now that I had the new baby. I barked at him about how the WHO recommends nursing for 2 years and as long as is mutually desired thereafter and that if I wanted parenting advice from him, I would have asked. He checked her from head to toe and quickly left the room!
Fast forward to this past February, I got a copy of her medical records and mine as well. I got her records to be able to get her social security card (she didn't get one in the hospital because she didn't have a name when we left). I got my records just for curiosity's sake. In both of our records, there is no mention of her ever having a problem with her heart rate and the only mention with the episiotomy is that tearing was likely. In her records, it very clearly states that her fetal heart tones were reassuring throughout. Her heart rate was never a problem, there was no need for the episiotomy, he gained my consent through lying to me before cutting me from my vagina down toward my anus.
All in all, I'm VERY happy that I was able to have my vaginal delivery. But I very much feel as though my entire birth experience was a form of emotional, and at times, physical rape. I can't watch a video of a woman giving birth, be it in a hospital or at home, without longing to be in labor with her again, to be able to have a do-over. I cry a lot when I think about it. I have a copy of "The Business of Being Born" from Netflix that's been in my possession for several months now that I've not been able to force myself to watch. I'm afraid of everything flooding back to me again. My little breechling is now 19 months old. I wasn't able to begin facing my birth experience with her until about 4 months ago. Sure, I've been "bragging" about it since I gave birth, but it wasn't until recently that I really allowed myself to feel the emotions.
Mike videotaped the birth. I watched it for the first time a month or so ago and I was a crying mess just by halfway through it. I got to the part where he cut the episiotomy and I heard the loud cry I made and it was like being on that hospital bed all over again. He didn't wait long enough for the numbing medication to set in before he took the tool to me and I FELT my flesh being cut open. I had blocked that out of my mind. The time on the video after she was born, I look like someone else. I don't see myself when I watch the video. I was shaking from the epidural and perhaps the adrenaline pumping through my body. I was completely detached from the entire situation. Mike was off near the table where they'd brought her to weigh her and clean her off and I was listening to all the conversations around me and adding babbling sentences to other people's conversations. I think the most telling part of the entire video and the entire story is that I didn't cry when she was born. When they placed her in my arms it was like I was holding A baby but not MY baby. I had no attachment to her whatsoever. I continued to feel like that for the first month or so of her life. I had this baby with her mouth on my nipple and I was changing her diapers and she was like this strange little alien that had just dropped from the sky and I was expected to take care of her.
Around the time she was able to start smiling and became more interactive with others around her, that's when I felt a bond and I *knew* she was mine and I felt that surge of love hormones. Before that time, I was just going through the motions. I knew she needed to eat so I offered my breast. I changed her diapers and her clothes, I bathed her, she slept next to me at night and I did all of the other things a mother does for her child and that I did for my first daughter but for that first period, I didn't feel as though I was doing these things for my own child. Knowing what I know now, I was in a state of shock after giving birth to her. I don't see myself in the video or in pictures because the self I've come to know and love after 20-some years on this planet was not really present. That "me" took a hike the moment the doctor came into the room and barked at me about how he would never take the kind of risk I was taking with his own child and he didn't understand why I would take it with mine. While I am very much bonded with my daughter now, and have been since she was around 2 months old, I feel as though now that I'm finally facing my birth experience head on, ugliness and all, I'm finally getting to know myself again, the self that ran away and hid when I got to the hospital that day.
In September of 2009, I made a choice to finally go to college, having graduated from high school in 2000. I think the reason I waited so long to go back to school is that I didn't know what I wanted to be when I grew up. Now I know I want to be a midwife. As of January 11, 2010, I will be attending classes to gain the general education credits necessary to enroll in the nursing program. The next step after becoming a nurse is to complete the training to become a certified nurse midwife. Through personal experience, I have found that there is a frighteningly MASSIVE amount of incorrect information out there for women who are pregnant, about to give birth, nursing a baby, a toddler and raising children in general. There are blanket statements passed around to women who, through no fault of their own, just don't know any better and believe that doctors (OBs and pediatricians specifically) are infallible. For a long time, I was one of those people. I felt that doctors were bound by their oath to "do no harm" and that if they'd gone to school for so long for their specific field, obviously they must be right. My experiences over the years have taught me otherwise. And I am grateful for those experiences and both of my daughters for the parts they have played.
Labels:
birth stories,
breech,
c-section,
cesarean,
epidural,
interventions
Friday, January 8, 2010
Washington Post article on breech birth

The woman featured in this article who had two cesareans for breech and then went on to have a breech VBAC is an ICAN chapter leader!
Breech is near and dear to me since a young woman contacted our chapter a year and half ago desperate for help with finding an OB to deliver her breech baby. I was at a loss. I knew of none at that time, except for homebirth midwives, who would or could. To tell this woman I couldn’t help her prevent this cesarean was devastating and I will never forget it. Fortunately, she went on to deliver vaginally in a hospital.
When I heard Canada was reversing its policy on breech it gave me hope. If other countries are changing their policies on birth, we may someday too. Every woman should be prepared. Breech is not abnormal, it is just another way for a baby to come out. So because of this, I do have hope that the US will practice more evidence-based medicine with birth in the hospitals. That one day the VBAC rate will be over 50% and the c-section rate well under 20%. We will see healthier moms and healthier babies, we all know that. It starts with us, trusting our bodies and choosing a professional who does as well, and who is skilled in more than just the knife.
Next post: Jamie's Breech Birth story!
Thursday, January 7, 2010
Emergency Childbirth, or common sense?
This was forwarded to me by another midwife - advice for impromptu birth attendants, straight from the DOD. It would be wonderful if medical practitioners routinely followed this commonsense advice for safe birth! Notice there is no mention of checking for a Cesarean scar first...
Emergency Childbirth Reference Guide Posted at 01:18 AM on January 06, 2010
U.S. Department of Defense
Emergency Childbirth
A Reference Guide for Students
Medical Self-Help Training
Course Lesson No. 11
Emergency Childbirth: What To Do
1. Let nature be your best helper. Childbirth is a very natural act.
2. At first signs of labor assign the best qualified person to remain with mother.
3. Be calm; reassure mother.
4. Place mother and attendant in the most protected place in the shelter.
5. Keep children and others away.
6. Keep hands as clean as possible
7. Keep hands away from birth canal
8. See the baby breathes well.
9. Place the baby face down across the mother's abdomen.
10. Keep baby warm.
11. Wrap afterbirth with baby.
12. Keep baby with mother constantly.
13. Make mother as comfortable as possible.
14. Identify baby.
What Not To Do
1. DO NOT hurry.
2. DO NOT pull on baby, let baby be born naturally.
3. DO NOT pull on the cord, let the placenta (afterbirth) come naturally.
4. DO NOT cut and tie the cord until the baby AND the afterbirth have been delivered.
5. DO NOT give medication.
DO NOT HURRY - LET NATURE TAKE HER COURSE.
{emphasis is not mine - I copied this exactly as written}
This is how I approach attending VBAC as a traditional midwife and it works quite well - just ask the mothers!
Emergency Childbirth Reference Guide Posted at 01:18 AM on January 06, 2010
U.S. Department of Defense
Emergency Childbirth
A Reference Guide for Students
Medical Self-Help Training
Course Lesson No. 11
Emergency Childbirth: What To Do
1. Let nature be your best helper. Childbirth is a very natural act.
2. At first signs of labor assign the best qualified person to remain with mother.
3. Be calm; reassure mother.
4. Place mother and attendant in the most protected place in the shelter.
5. Keep children and others away.
6. Keep hands as clean as possible
7. Keep hands away from birth canal
8. See the baby breathes well.
9. Place the baby face down across the mother's abdomen.
10. Keep baby warm.
11. Wrap afterbirth with baby.
12. Keep baby with mother constantly.
13. Make mother as comfortable as possible.
14. Identify baby.
What Not To Do
1. DO NOT hurry.
2. DO NOT pull on baby, let baby be born naturally.
3. DO NOT pull on the cord, let the placenta (afterbirth) come naturally.
4. DO NOT cut and tie the cord until the baby AND the afterbirth have been delivered.
5. DO NOT give medication.
DO NOT HURRY - LET NATURE TAKE HER COURSE.
{emphasis is not mine - I copied this exactly as written}
This is how I approach attending VBAC as a traditional midwife and it works quite well - just ask the mothers!
Tuesday, January 5, 2010
Twin Cities Metro Cesarean/Vaginal Birth Rates
One of the latest things going around our birth advocacy community is the 2008 cesarean and vaginal birth rates for the Twin Cities metro hospitals. As many of us in ICAN have learned - it's important to consider these rates when giving birth. Just as it's important to consider your provider's individual numbers as well. I was kind of saddened to learn that Unity's c-section rate (where I had my cesarean) was on the low end. I guess I still kind of wish that my induction for pre-eclampsia would have worked out.
Those of us who have had a VBAC or are preparing for a VBAC are considering where to give birth. For those of us who decide that it will be hospital, these rates should be very helpful in deciding where to give birth. A friend of mine just became pregnant for the first time and who did she call right away? Me - and believe me, I do feel honored. She called me because ever since my baby #1 came I've been very vocal about birth - go figure. In just one night I got her thinking about midwifery care, and then after emailing her some information, I got her focused on the East Metro hospitals (minus United) instead of Abbott. All this before this handy little spreadsheet came out:
When looking at these numbers - it's important to consider the cesarean vs. vaginal birth rates. Obviously the higher the c-section rate - the more likely your chances are of having one. That is why it is important to know your provider's c-section rates, vaginal birth rates, VBAC success rates. The World Health Organization recommends a c-section rate no higher than 10-15% to keep the surgeries from doing more harm than good. Only one of our hospitals actually measures up to that - so that's a whole other post, but consider these rates and may you use it to ask questions of your providers, do research before deciding where you are going to birth. I had my VBAC at U of M Fairview, Riverside. They are on the higher end for the metro c-section rates, however, my midwife group had an 85-90% success rate for VBAC deliveries. That number was definitely a factor in helping me choose those particular providers. It all goes back to making an informed decision. Hopefully this will be another piece towards helping women make informed decisions.
Monday, January 4, 2010
Childbirth turns tragic, then joyful—a Christmas Miracle! or The Dangers of Epidurals?
 Alarm bells went off when I read this amazing story of a mom and her baby miraculously coming back to life after “mysteriously” dying during childbirth. I knew there had be some reason her heart stopped (like all the drugs?!) I couldn’t find it though—the doctor kept on reiterating what a mystery it all was.
Alarm bells went off when I read this amazing story of a mom and her baby miraculously coming back to life after “mysteriously” dying during childbirth. I knew there had be some reason her heart stopped (like all the drugs?!) I couldn’t find it though—the doctor kept on reiterating what a mystery it all was.Well, turns out she was induced and had an epidural. So why wasn’t any of this mentioned in the media or by the doctors involved? Have these things become such a common part of birth that no one even thinks of them as unnatural? I am totally baffled and appalled.
Henci Goer explained how epidurals can cause cardiac arrest in a blog post this week:
Her Survival Was a “Christmas Miracle,” but the Disaster Was Man-Made
Every woman needs to know all the facts. When I voiced my concerns for the epidural to my OB, he patted my knee and said “of course you will have it!” The same way he patted my knee and said I would have a repeat c-section instead of a VBAC for any subsequent births……
My point to this is not that epidurals are across the board wrong or bad. They can be very helpful when someone is at their breaking point, too tired, too scared, or in my case pumped full or Cytotec and Pitocin and totally unable to handle the pain. Everyone should be able to decide if it is time. But we need to know the risks! We have a right to know the risks. We deserve to know that it isn’t a miracle cure that will make childbirth a piece of cake.
And maybe we should be really alarmed that a doctor made no mention of this when she said her patient's death was a mystery.
I am glad she and the baby survived, but as a birth activist, a VBACtivist, the end does not justify the means. Our experiences matter.
Subscribe to:
Posts (Atom)
